Menopause is a natural phase in a woman’s life that comes with various physical and emotional changes. At Naina Homeo Care, we offer Menopause homoeopathic treatment in Lucknow, UP, to help women manage menopause symptoms effectively and naturally. Our approach focuses on understanding your unique symptoms and providing remedies that address your needs without side effects.
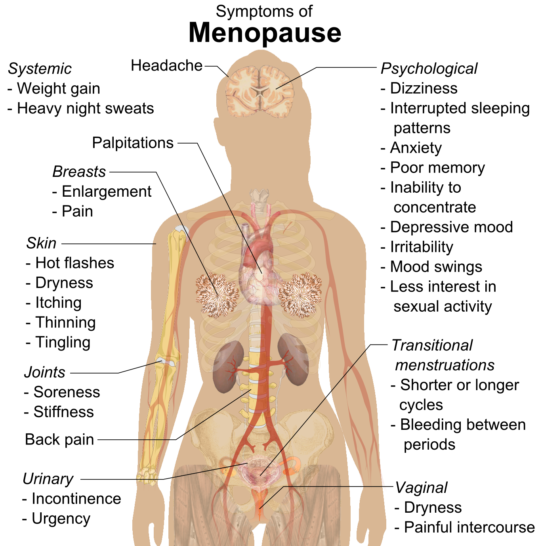
Menopause can bring a range of symptoms, such as hot flashes, mood swings, sleep disturbances, and fatigue. These changes can be overwhelming, affecting both your physical and mental well-being. At Naina Homeo Care, we believe in a holistic approach that treats the root cause of these symptoms rather than just offering temporary relief.
Homeopathy works gently to balance your hormones and ease the transition, making this stage of life smoother and more comfortable.
Our experienced homoeopathic doctor will take the time to understand your complete medical history, lifestyle, and specific symptoms before suggesting a treatment plan.
The remedies are tailored to support your body’s natural healing process, helping you regain balance and well-being. Homeopathy is safe, natural, and free from harmful chemicals, making it an ideal option for long-term health management. In addition to providing remedies, we guide lifestyle changes, diet improvements, and stress management techniques that complement the treatment.
This comprehensive care ensures that you not only find relief from menopause symptoms but also maintain overall good health during this phase of life. At Naina Homeo Care, we offer compassionate care focusing on treating the individual as a whole.
If you are struggling with menopause symptoms and seeking a natural solution, visit us for a personalized homoeopathic consultation. We are here to help you navigate this transition quickly and confidently, providing you with the care and support you deserve.
Complications may occur soon after menopause or may develop late as sequel of prolonged oestrogen deficiency.
Genetic: Ten to twenty percent of premature menopause occurs in sex chromosome abnormalities. In 30 to 60 percent, autoimmune diseases such as mumps, thyroid dysfunction, hypoparathyroidism, addison’s disease are present.
Radiation menopause depends upon its dosage. Some recover from amenorrhoea in a year or so. Alkalytic drugs are storng inducers of premature menopause.
premature menopause can induce menopausal symptoms and complications much earlier and in a severe form. A cause needs to be elucidated and treated.
All © Copyright Rights Reserved by Naina Homeo Care. Designed by Web Cloud Technology